PRESS RELEASE | New audio play, TISSUES.WATER.CLOCK., shines a light on hidden illnesses
Invisible ME, a Cornwall-based support network for Myalgic Encephalomyelitis / Chronic Fatigue Syndrome (ME/CFS) sufferers, has produced a new audio play exploring the experience of living with a life-changing illness.
TISSUES.WATER.CLOCK. is an audio play inspired by the stories and experiences of ME sufferers, carers and health professionals in East Cornwall which, together with an illustrated exhibition, profiles first-hand experiences of this unpredictable and often-misunderstood illness.
Invisible ME received funding from the National Lottery, FEAST and other charities to develop the unique dramatic work about a couple navigating everyday life with ME.
The idea for a play was originally conceived by producer and arts educator David Oddie and then developed by writer Jayne Newton-Chance, director Natasha Buckley and actors Jo Loyn and Paul Morel with Invisible ME co-founder Dr Hilary Doe as medical adviser.
The team of creative artists worked closely with participants to gather personal recollections and create both a play and a travelling exhibition – including a series of insightful and humorous illustrations by artist Tanya Morel.
The play comes at a pivotal time; on 1 April 2021, over 1 million people had reported experiencing Long COVID – symptoms persisting more than four weeks after the first suspected coronavirus (COVID-19) episode that are not explained by something else (source: ons.gov.uk). For some, the symptoms resemble those experienced with ME/CFS and it is expected that there will be a rise in cases of ME/CFS following the pandemic.
David Oddie said: “The process provided an informed platform to create a unique and authentic theatre piece bearing witness to the lives of ME/CFS sufferers, serving also as a metaphor for other ‘hidden’ illnesses and conditions.”
The original production conveying the reality of living with ME/CFS was initially scheduled for Autumn 2020. With the first lockdown delaying tour dates and ongoing Covid-19 restrictions, the likelihood of venues re-opening their doors for performances became uncertain. Consequently, the play was reimagined from a live theatre piece to a freely distributed audio drama intended to raise awareness, bear witness and communicate the lived experience of people affected by ME/CFS.
Dr Hilary Doe, Co-founder, Invisible ME, said: “It can only be hoped that we emerge from this experience with greater openness, compassion and understanding for people living with hidden illnesses, such as ME/CFS, to give a glimmer of hope for the 250,000 people who live with the condition in the UK.”
Extract: “…at the beginning of all this, when I didn’t know what it was, I used to worry that I was dying. And now, you know what? On the very, very bleakest days I worry that I’m not dying […] And then I get up, I get over it, I get on. Because that’s what we do. We do what we can when we can. We learn to smell the roses. We learn how to love better. We learn how to appreciate what we have…”
– Rachel, TISSUES.WATER.CLOCK.
About ME
ME/CFS is a debilitating disease classified as a neurological illness by the World Health Organisation. Its causes are not understood and the lack of a specific diagnostic test makes diagnosis difficult. Sufferers show a range of symptoms and its impact on their lives is profound. At the very severe end of the scale, sufferers are house or even bed-bound. At a more moderate level, sufferers can have their previous activity levels reduced by 50% or more. The challenges of people living with ME/CFS include gaining a diagnosis, lack of evidence-based treatment, and, most significantly, disbelief – even within families and sometimes the medical profession. The condition profoundly affects the health and lives of sufferers for many months, years or decades.
The play is available to stream on the Invisible ME website.
Listen now: invisibleme.org.uk
For interviews and further information on TISSUES.WATER.CLOCK, the accompanying exhibition or Invisible ME, contact David Oddie on:
01579 370642 /invisiblemecornwall@gmail.com
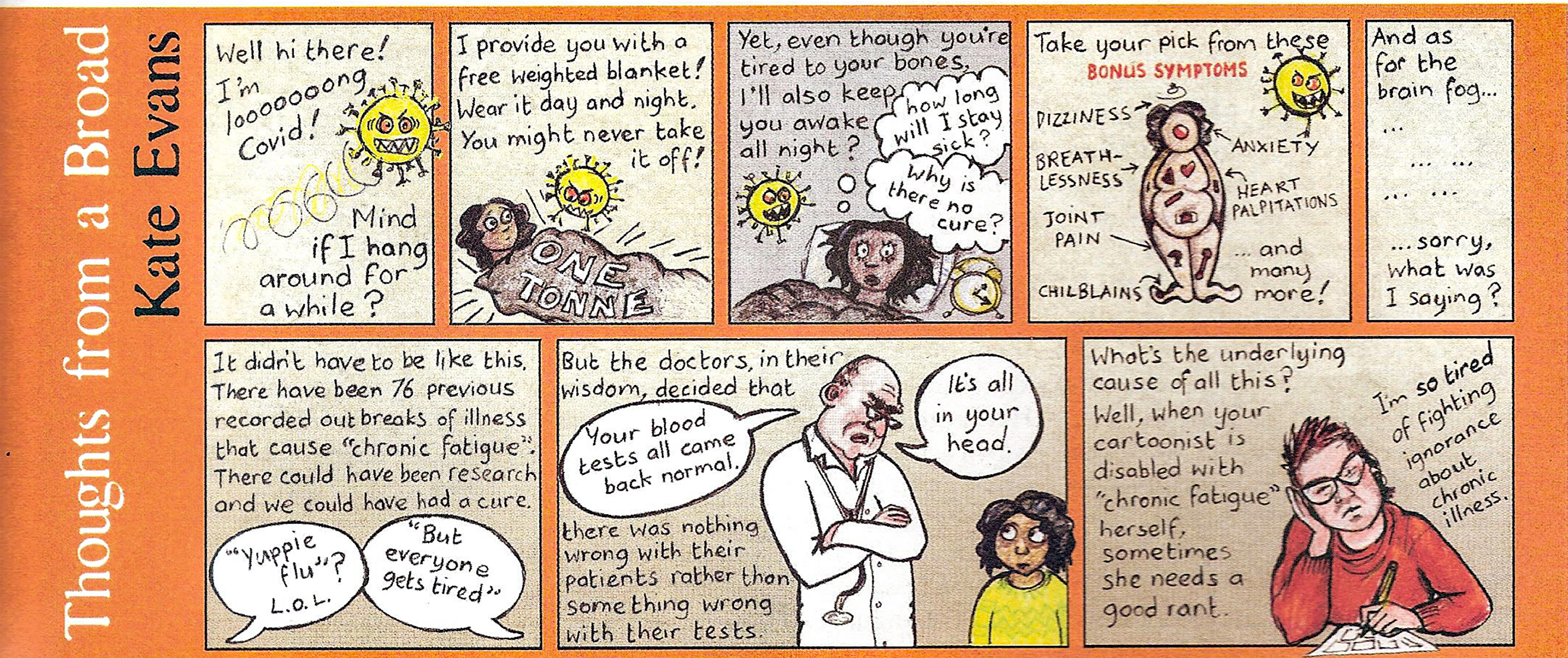
Cartoon that appeared in the April edition of the New Internationalist Magazine.
Feb 2021 update
There is an excellent article by George Monbiot in the Guardian which we would recommend warmly. He has really done his research and includes some moving testimonies which could have come straight from our exhibition and your own testimonies! This is the link: https://www.theguardian.com/commentisfree/2021/jan/21/were-about-to-see-a-wave-of-long-covid-when-will-ministers-take-it-seriously
Unfortunately we have had to postpone the play recording yet again because the studio we are using cannot guarantee a fully Covid free space for the session at this time. We will just have to be patient and hope we can get both the recording done and the Invisible ME exhibition on the road before too long. It’s frustrating because we are all ready to go!
Do please remember that we are still here and do get in touch if we can be of any help for a chat or whatever might be useful: we ain’t going anywhere and you are all very much in our thoughts.
Best wishes
David and Hilary
Feb 2021
TEMPLATE LETTER TO YOUR GP
Sufferers from ME/CFS have been struggling to be included on the ‘group 6’ list for Covid vaccinations. HIlary has therefore adapted a template, created by the ME Association, to help put the case to people’s surgeries. The strategy has proved to be effective in a number of cases.
PLEASE MODIFY IT TO SUIT YOUR PARTICULAR CIRCUMSTANCES.
THEN COPY AND PASTE TO YOUR OWN LETTERHEAD OR EMAIL.
MAKE SURE IT’S DATED AND SIGNED, CONTAINS YOUR HOME ADDRESS AND DATE OF BIRTH –THEN EITHER EMAIL IT OR SEND BY ROYAL MAIL
Dear XXXX,
I am writing to ascertain if, due to having ME/CFS, I have been added to the ‘group 6’ list for Covid vaccinations. The ME Association (MEA) has advised people with ME/CFS to check this with their GP surgeries, as not all GP surgeries have been adding people with ME/CFS to group 6 of the JCVI priority list.
The MEA has also provided the following background information for health professionals and has confirmed that people with ME/CFS are reporting that they have been placed in group 6 as a result of receiving this information.
1 People with a chronic neurological disease are listed as having an underlying health condition in group 6 in the JCVI guidance. See page 9 in Chapter 14a of the ‘green Book’ guidance on Covid vaccine:
2 Both the World Health Organisation (in ICD10 section G93.3) and NHS England classify ME/CFS as a neurological disease:
3 Even though ME/CFS is not included as a specific disease in the ‘green book’ list of neurological conditions, the guidance makes it clear that the list is not exhaustive.
4 The ‘green book’ guidance (page 10) states that: The examples above are not exhaustive, and, within these groups, the prescriber should apply clinical judgment to take into account the risk of COVID-19 exacerbating any underlying disease that a patient may have, as well as the risk of serious illness from COVID-19 itself.
5 New infections are probably the commonest cause of exacerbation or relapse of ME/CFS – as noted in section 3.3.2 of the Chief Medical Officer’s Working Group Report on ME/CFS: https://meassociation.org.uk/wp-content/uploads/CMO-Report-2002.pdf and in section 1.6.4 of the new (draft) NICE guideline on ME/CFS which will become operational in April 2021:
https://www.nice.org.uk/guidance/gid-ng10091/documents/draft-guideline
6 Patient evidence to the MEA also indicates that almost everyone with ME/CFS who has caught COVID-19 has had a significant and/or prolonged relapse of their ME/CFS. This is not surprising given the considerable degree of clinical overlap between ME/CFS and Long Covid. I would therefore be very grateful if you could confirm that I have been added to the Group 6 list.
To ensure that I can be contacted as soon as I am eligible, please add my mobile number to my file to be contacted by this, if not already saved there. Thank you very much in advance for your time and indeed for everything you and your other NHS colleagues are doing during this pandemic.
Kind regards,
Full name
Address
Date of birth
Update letter to Invisible ME participants August 2020.
On Sunday the 26th July the writer Jemma Kennedy wrote a moving article for the Observer/Guardian newspaper about her lack of recovery from the C-19 illness. She made important links between her experience and that of ‘our first cousins’, people living with ME/CFS and the devastating impact of that condition on their lives. You can see the article here:
In response we wrote a letter to the Observer/Guardian highlighting the points Jemma made i.e. the issues of lack of cure, diagnosis, treatment and disbelief faced by people with ME/CFS and we expressed the hope that the increase in the number of people displaying Post Viral Syndrome following C-19 might lead to great understanding and awareness of the reality of ME/CFS. We are pleased to say the Observer published our letter (see below) in their letters section on Sunday 2nd August. We are attaching a copy of the letter with this e-mail for you to read.
On related issues we are now hoping our new play about ME/CFS will be undertaking a pilot tour in March 2021. This of course depends on the state of play regarding C-19 and the ever changing rules on lockdown. Preparations are well underway for the exhibition and we plan now for that to be available before Christmas. Tanya Morel’s series of supporting pictures are very powerful and also humorous, which we hope will encourage people to look further at the content.
Love and best wishes to you all and do remember we are still here if you would like to call us or get in touch.
David and Hilary
Observer letter
In her excellent article, ‘I’m a Covid-19 long hauler’ (26th July) Jemma Kennedy writes movingly about her ongoing symptoms following the illness and makes connections with the experience of ‘our first cousins’ whose lives have been devastated by the much misunderstood illness ME/CFS (Myalgic Encephalomyelitis/Chronic Fatigue Syndrome). This condition profoundly affects the health and lives of sufferers for many months, years or decades.
Jemma identifies the profound challenges of people living with ME/CFS, for example, in gaining a diagnosis, the lack of an evidenced base treatment, and, most significantly, the disbelief – even within families and sometimes the medical profession. This latter can lead to isolation and despair.
There are several reports now documenting how some patients with Covid-19 have developed symptoms of Post Viral Fatigue Syndrome and have been unable to return to their normal health. These symptoms resemble those experienced with ME/CFS and it is expected that there will be a rise in cases of ME/CFS following the pandemic.
Covid-!9 has been an unrelenting nightmare for too many people but if we emerge form the experience with a greater openness, compassion and understanding for people living with related ‘hidden’ illnesses such as ME/CFS then that would be a silver lining, a glimmer of hope for the 250,000 people who live with the condition in the UK.
Dr Hilary Doe
David Oddie
GOOD NEWS!
An ambitious genetic study into ME/CFS has received 3.2 million pounds from the Medical Research council and the National Institute for Health Research. Researchers will be collecting samples from 20,000 people. The aim is to develop diagnostic tests and targeted treatments by identifying differences in people’s DNA that may affect their risk of developing ME/CFS and reveal underlying causes. Lead researcher Prof Chris Ponting said, ‘we hope to transform ME/CFS research by injecting much needed robust evidence into the field’.
This article in today’s Guardian summarises the project:
You can offer to volunteer for the project by signing in on the project web-site:
The project is exciting as it may help to identify and uncover the biological root of ME/CFS. Let’s support it!
This poem was sent to us by a participant in the network.
Pandemic Poem
What if you thought of it
as the Jews consider the Sabbath—
the most sacred of times?
Cease from travel.
Cease from buying and selling.
Give up, just for now,
on trying to make the world
different than it is.
Sing. Pray. Touch only those
to whom you commit your life.
Center down.
And when your body has become still,
reach out with your heart.
Know that we are connected
in ways that are terrifying and beautiful.
(You could hardly deny it now.)
Know that our lives
are in one another’s hands.
(Surely, that has come clear.)
Do not reach out your hands.
Reach out your heart.
Reach out your words.
Reach out all the tendrils
of compassion that move, invisibly,
where we cannot touch.
Promise this world your love–
for better or for worse,
in sickness and in health,
so long as we all shall live.
This is a poem written by a member of the Invisible ME network who wishes to remain anonymous:
ME
shall I be angry or shall I cry
child of mine
such weary exhaustion
total exhaustion
every muscle aches
waves of nausea
you struggle to nourish your self
I see you shielding eyes from bright light
you keep curtains drawn
so weary at 15… I want to cry
too tired with helping you
like a frail old person
you creep slowly up the stairs
friends too great an effort
you become shielded, guarded
and your own intense energy has hidden itself
waiting hoping longing
it takes a long time
you learn through sorrow
to listen to the emotion of your body
and muscles of body knowing
desire slowly emerges
and I still want to cry for those years
hard times of lonely aloneness for us both
It has left you deeply aware
life is very precious and can be precarious
breath in and breath out
Gratitude
We asked for ideas about what it is like to have ME/CFS: This is D’s response:
Remember what it’s like to have Flu? Man-Flu in particular (an especially aggressive variant, and DEFINITELY a real thing). Your tongue feels like it’s made of carpet, your body temperature fluctuates uncontrollably and your head is full of some sort of low-grade cement? Your taste buds function only in so much as to make everything you consume taste like recycled cardboard, your ears are apparently full of fibre glass and you have the ghostly pallor of someone who’s spent 6 months living in a box in an arctic forest? Your limbs ache, you can barely form a coherent sentence and worst of all, you have such inexorable fatigue that a trip to the bathroom feels like the final approach to the summit of Everest.

Remember that illness? Maybe it wasn’t Flu. Perhaps it was Mumps, Glandular Fever or Pneumonia. Possibly you were recovering from a bout of surgery, with all the attendant post-operative aches and pains?
Now try and imagine that instead of this unhappy state of mind and body dissipating after a week or two, the fatigue stays with you. Often, and unpredictably, some of the other symptoms also spontaneously reappear. Some mornings, you struggle to put words together. A journey upstairs leaves you breathless and bewildered. You read the same page of a book 6 times before you realise it hasn’t gone in, and after 15 minutes focusing on something as simple as reading, your daily reserves of mental energy are completely exhausted. A brief stroll to the shops, or perhaps a walk to the park with your children or grandchildren FEELS like the natural thing to do, but once the endorphins wear off, even these modest achievements might entail a day or more in bed recovering from the sheer tiredness precipitated, along with all of the attendant aches and pains outlined above. Headaches come and go; appetite fluctuates, and sometimes for no discernible reason mealtimes swiftly result in the worst exigencies of Irritable Bowel Syndrome (a condition that sounds amusing until you’ve experienced it).

And this goes on for weeks, months, years, until understandably the sufferer may begin feeling more than a tad depressed about their situation. Work becomes untenable, as the sheer physical effort of maintaining anything like an alert or professional presence becomes impossible. Social relationships become difficult as the multiplicity of symptoms hold sway. Worst of all, perhaps, imagine that not only are you suffering from such a bewildering and impactful suite of symptoms, but compounding your misery, many of those purportedly empowered to assist you are openly cynical about the provenance of your illness. As there is no singe test for the condition, a differential diagnosis can take literally years to achieve, and even this is contingent on the degree of awareness and understanding exhibited by your General Practitioner. Despite feeling like you’re perpetually wading through treacle, you may be told by these and other professionals that you need to exercise more, or even that the condition is entirely in your head.
Derogatory epithets applied to your illness for years, like “Yuppie Flu”, mean that there is such cynicism abroad in the culture pertaining to your illness that friends and even family may become exasperated and offer little sympathy or understanding, despite clinical studies showing that those experiencing your condition have “…the lowest health-related quality of life score when compared to cancer, diabetes, lupus, stroke, heart disease and chronic renal failure”. Sometimes, faced with this multi-headed Hydra of sickness and disbelief, you may even begin to doubt yourself, compounding the negative emotions already prevalent as you battle through each day to achieve some sort of equilibrium.

Sadly this condition is not some grim fiction, but a lived reality for many of the hundreds of thousands of sufferers battling ME (Myalgic Encephalomyelitis) in the community. Aspects of it have been my reality for some years. It is of the utmost importance to me that ordinary people understand the devastating impact of this very real condition on sufferers, and that professionals, most particularly within the Health, Benefit and Social Care systems, are imbued with sufficient understanding to treat sufferers with the respect they deserve commensurate with the severity of their condition. I remember the personal affirmation I received when I finally felt acknowledged and believed by healthcare professionals; Given the daily struggle outlined above, sometimes battling through life is an overwhelming task in itself, without the additional and enervating prospect of having to convince others, especially when they should know better. Under these circumstances, to quote Joseph Conrad, “The question is not how to get cured, but how to live.” As a cure still looks like a distant prospect, this is the challenge all ME sufferers face, and a major part of the solution is making the invisible, visible.
This is what S. said:
Yesterday I drove 5 miles to the vet with our injured cat because my husband, who has cancer related fatigue, was unable to drive. It was a short visit and I drove straight back. On returning home I went to bed and stayed there resting and sleeping until this morning. This is typical of how my body responds to activity. I can drive only once or occasionally twice a week and then for only very short journeys usually only a couple of miles. I am short rations of energy and can only use it once.

My body like a car sitting on your drive that has the potential to take you anywhere but with only a litre of petrol in the tank each day that can’t be saved to use another day. Friends say “But your car looks fine, it must be capable of going anywhere you want to go. It must be that you don’t really want to go any further.” It is frustrating and distressing to be disbelieved, no-one can see the pain and the widespread prejudice surrounding ME is a cause of isolation and depression. Please bear in mind that scepticism about the condition deflates us like a balloon; we think “Here we go again, I am up against it again.” Trying to explain is extremely tiring and dispiriting . It is not just strangers; even my own family scoffed and called me a benefit fraud.
It is not just my body that is effected, brain fog is a major problem for me. Along with poor balance, too much effort causes tremor. I am over-sensitive to light, sound and smells. Answering questions is difficult for me and I can be slow to respond, so interviews are stressful. When ME hit me nearly 20 years ago felt as if old-age had come to meet me, at the age of 46 my active life was largely over and that is how it has been.
THE OPEN MEDICINE FOUNDATION
The Open Medicine Foundation ran a poetry competition for which there were many contributions. The winning poem was:
Even Though
By Laurie Glass
Even though we’re sick, in pain,
and our bodies feel so drained,
we feel the agony unfold,
our lives are put on hold,
we keep our inner strength.
Even though we’ve gone away,
and we’re missing ev’ry day,
we feel we’re on our own,
yet know we aren’t alone,
together we are stronger.
Even though we’ve all been wronged,
we’ve been ignored for oh, so long,
for years we’ve been denied,
our needs were set aside,
we are grateful things are changing.
Even though we’ve been unheard,
others help us spread the word,
together we’re unstoppable,
we’re making changes possible.
We’ll never stop trying.
Even though we are in tears,
grieve the loss of many years,
experts work on our behalf,
to try to get us back.
We’re grateful for each one.
Even though our hearts are breakin’,
even though our lives were taken,
we try to keep on dreaming,
we try to keep believing
that better days will come.
The poem was made into a song ‘Keeping the Hope’ by Maxwell Elefant and 95 North. You can find it here:
https://www.omf.ngo/2019/05/22/keeping-the-hope-song-release/
